Introduction
Understanding the complexities of medical billing for post-acute care is crucial in today’s healthcare industry. Post-acute care includes specialized services provided to patients after they have been discharged from a hospital, including home health care, skilled nursing, rehabilitation, and hospice care. This article will provide complete insights into post-acute care billing, ensuring that billing processes are not only compliant but also optimized for accuracy and reimbursement. Whether you’re a healthcare provider, billing specialist, or administrator, having a firm hold of these workings will give you the confidence to effectively manage post-acute care billing.
What is Post-Acute Care?
Post-acute care is a critical component of the healthcare range, aimed at helping patients recover and regain independence after an acute illness or surgery. It typically follows a hospital stay and includes services such as physical therapy, occupational therapy, speech therapy, and skilled nursing care.
Patients requiring post-acute care often have complex needs, which makes accurate medical billing even more essential. Billing for these services must account for the specific types of care provided, the duration of the services, and the individual patient’s condition.
Importance of Accurate Post-Acute Care Medical Billing
Accurate medical billing in post-acute care is crucial for several reasons. First, it ensures that healthcare providers are reimbursed for the services they provide. Without accurate billing, providers risk not getting paid, which can affect their ability to offer quality care.
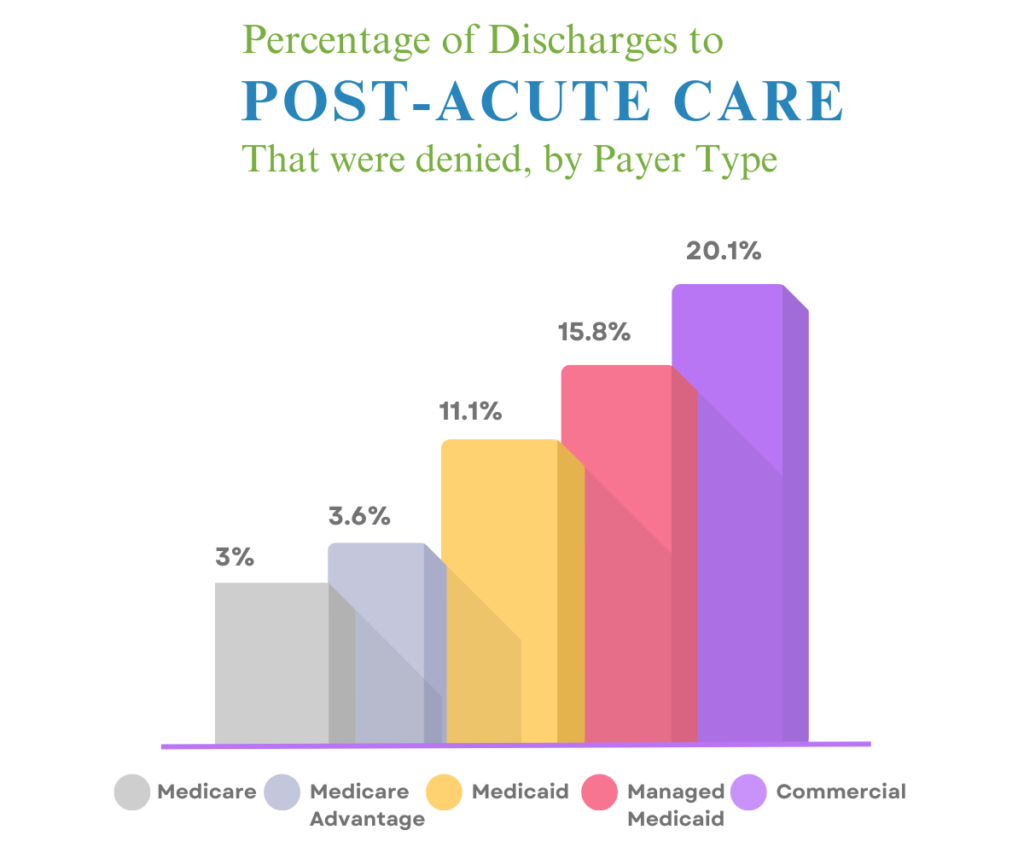
Moreover, accurate billing is essential for maintaining compliance with healthcare regulations. Post-acute care providers must adhere to strict guidelines set by payers, including Medicare, Medicaid, and private insurers. Failure to comply with these guidelines can result in claim denials, delays in payment, or even legal consequences.
Key Components of Medical Billing for Post-Acute Care
Medical billing for post-acute care involves several key components that must be accurately managed to ensure accuracy and compliance:
- Patient Information: Accurate collection and verification of patient demographic information are fundamental to medical billing success. This includes details like name, address, insurance information, and the type of post-acute care received.
- Coding: The use of standardized codes, such as ICD-10 (International Classification of Diseases) and CPT (Current Procedural Terminology), is critical in post-acute care medical billing. Proper coding ensures that services are accurately represented and that providers are reimbursed appropriately.
- Documentation: Thorough and accurate documentation of the care provided is essential for justifying the billing codes used. This includes detailed records of the services reduced, the duration of care, and the outcomes achieved.
- Claims Submission: Once the billing information is compiled, claims must be submitted to the appropriate payer. This process requires attention to detail to ensure that claims are not rejected due to errors or oversights.
Understanding ICD-10 and CPT Coding in Post-Acute Care
ICD-10 and CPT coding are two critical components of medical billing that play a important role in post-acute care:
- ICD-10 Coding: ICD-10 codes are used to classify and code all diagnoses, symptoms, and procedures recorded in combination with hospital care in the United States. In post-acute care, these codes are used to document the patient’s medical condition and the necessity for the services provided. Accurate ICD-10 coding is essential for justifying the need for post-acute care and ensuring that claims are processed correctly.
- CPT Coding: CPT codes are used to describe the specific medical procedures and services performed by healthcare providers. In post-acute care, CPT codes are used to detail the exact nature of the care provided, whether it’s physical therapy, nursing care, or other rehabilitative services. Proper use of CPT codes is essential for securing reimbursement and avoiding claim denials.
Challenges in Medical Billing for Post-Acute Care
- Medical billing for post-acute care presents unique challenges, such as:
- Complexity of Care: Patients in post-acute care often have complex needs, which can make coding and billing more complicated. Accurately documenting and coding these services requires specialized knowledge and attention to detail.
- Regulatory Compliance: Post-acute care providers must follow many regulations set forth by government agencies and private payers. Staying compliant with these regulations while ensuring accurate billing can be challenging.
- Claim Denials: Denials are a common issue in post-acute care billing. They can occur for various reasons, including coding errors, insufficient documentation, or failure to meet payer guidelines. Handling these denials efficiently is critical to maintaining revenue flow.
Best Practices for Medical Billing in Post-Acute Care
To navigate the complexities of medical billing in post-acute care, it is essential to implement best practices that can streamline the process and minimize errors:
- Regular Training: Ensure that billing staff is regularly trained on the latest coding standards, regulatory changes, and payer requirements. Continuous education is key to maintaining medical billing accuracy.
- Thorough Documentation: Encourage healthcare providers to document all services in detail. Comprehensive documentation supports the coding process and reduces the risk of claim denials.
- Pre-Bill Audits: Conducting pre-bill audits can help identify potential errors before claims are submitted. This practical approach can reduce the number of denials and improve overall billing efficiency.
- Use of Technology: Invest in billing software that can automate parts of the medical billing process, such as code selection and claims submission. Automation can reduce the risk of human error and improve the speed of claim processing.
The Role of Electronic Health Records (EHR) in Post-Acute Care Billing
Electronic Health Records (EHR) enhance the accuracy and efficiency of medical billing in post-acute care. EHR systems allow for seamless integration of patient data, which is essential for accurate billing. These systems can automatically populate billing forms with the necessary codes based on the documentation entered by healthcare providers.
Moreover, EHR systems can track patient progress, store detailed care records, and ensure that all required documentation is complete and accurate. By reducing the possibility of errors, EHRs help ensure that billing is accurate and compliant with payer requirements.
Navigating Medicare and Medicaid Billing for Post-Acute Care
Medicare and Medicaid are two of the largest payers for post-acute care services. Understanding the billing requirements for these programs is important for successful reimbursement:
- Medicare Billing: Medicare provides coverage for various post-acute care services, including home health care, skilled nursing facility (SNF) care, and inpatient rehabilitation. Each type of service has specific billing requirements, including the use of specific codes and documentation standards.
- Medicaid Billing: Medicaid coverage varies by state, and each state has its own set of rules and regulations for billing post-acute care services. Providers must be familiar with their state’s Medicaid program to ensure compliance and proper reimbursement.
Strategies to Reduce Claim Denials in Post-Acute Care Billing
Reducing claim denials is a top priority for any healthcare provider, and post-acute care is no exception. Here are some strategies to minimize denials:
- Accurate Coding: Ensure that all services are accurately coded using the correct ICD-10 and CPT codes. This reduces the risk of denials due to coding errors.
- Complete Documentation: Incomplete documentation is a common reason for claim denials. Make sure that all necessary details are documented to support the services provided.
- Timely Submission: Submit claims as soon as possible after services are reduced. Delayed submissions can lead to denials or delayed payments.
- Regular Audits: Conduct regular audits of your medical billing processes to identify and correct any issues that could lead to denials.
Future Trends in Post-Acute Care Billing
The field of post-acute care billing is continuously developing, with new trends emerging that can impact how billing is conducted:
- Value-Based Care Models: As healthcare shifts towards value-based care, post-acute care providers will need to adapt their medical billing practices to align with these models. This may involve new coding practices and a focus on outcomes-based reimbursement.
- Advanced Analytics: The use of advanced analytics in medical billing is growing. These tools allow providers to identify trends, anticipate denials, and optimize billing processes. Leveraging these tools can lead to more efficient and accurate billing.
Conclusion
Medical billing for post-acute care is a complex yet essential part of the healthcare industry. Healthcare providers need to understand key aspects of medical billing, such as accurate coding and compliance with regulations, to ensure proper reimbursement for the important services they provide. Implementing best practices and staying informed about industry trends will improve the efficiency and accuracy of medical billing processes, Secure MSO ultimately providing high-quality post-acute care medical billing services.